Q and A with Tovia Smith, MD : Urogynecologist : Virginia Women’s Center located in Richmond, VA
Dr. Tovia smith focuses on pelvic floor disorders, such as pelvic organ prolapse, urinary incontinence, and accidental bowel leaking.
http://www.virginiawomenscenter.com/staff-tovia-m-smith-md.html
Q: How can we make sure postpartum care is more than a few checkups?
A: The USA is actually incredibly behind. In Europe, healthcare automatically provides for pelvic floor checkups. In the USA, a woman receives a 6 week checkup follow up appointment that encompasses the infant and breastfeeding (this is generally referred to as the breast, breastfeeding, and bottoms checkup).
If a woman has had a third or fourth degree sphincter tear, she should be referred as soon as possible for a surgical repair.
Suggestion: Use Miralax following delivery to avoid constipation that is often caused by the iron in postpartum vitamins.

Q: I’ve been using oral birth control since I was 17. Now, I’m in my 50’s and menopausal, experiencing heat flashes and other discomfort so I must go on HRT. How safe is it to be on HRT?
A: Views on Hormone replacement therapy are very controversial. A woman must analyze the risks and benefits and changes in her quality of life, in addition to her pre-standing risk for breast cancer prior to deciding whether to continue.
Q: If I need long term birth control, what is the best solution?
A: There are many long term birth control methods. Studies from the 70’s gave IUD’s a bad reputation because of the theory of risk for increased rate of pelvic inflammatory disease. IUD’s are actually very safe. Tubal ligation and vasectomy are great hormone free options.
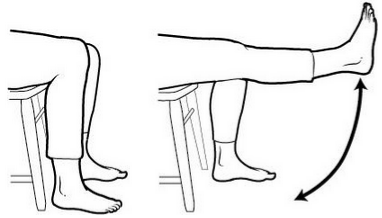
Q: What are the safest forms of exercise for someone with sciatica?
A: Pelvic floor and core stabilization exercises are perfectly safe, in addition to anything “symmetrical.” Avoid running or elliptical, for example. Many very fit patients have pelvic floor issues or are not aware that they have a weakness.

Q: How can I improve my quality of life following mesh surgery?
A: Native tissue repairs have 20% reoccurrence rate of pelvic prolapse. Mesh surgeries began when surgeons began using the same mesh used for hernias in the vaginal walls. This fails because abdominal walls do not function in the same way. Mesh often can cause chronic pain and affect nerve functioning. It is particularly hard to remove, even with multiple surgeries, because it is designed to be incorporated into the body.
Treatment following mesh surgery requires “all hands on deck,” including pain management, surgeons, and physical therapy.
Physical therapy treatment options include muscle relaxation, dry needling, massage, etc.
Q: If I don’t have I.C. (interstitial cystitis), would there be any other reason for feeling the urge to urinate consistently?
 A: I.C. means a patient is consistently trying to achieve an empty bladder. This patient generally believes she has consistent UTI’s but no evidence of infection, bladder cancer, etc. This is a diagnosis of exclusion because many times the problem can only be identified by the treatments that don’t work. For example, I can exclude the possibility of overactive bladder syndrome if I prescribe antihistamines at night time and it doesn’t improve symptoms.
A: I.C. means a patient is consistently trying to achieve an empty bladder. This patient generally believes she has consistent UTI’s but no evidence of infection, bladder cancer, etc. This is a diagnosis of exclusion because many times the problem can only be identified by the treatments that don’t work. For example, I can exclude the possibility of overactive bladder syndrome if I prescribe antihistamines at night time and it doesn’t improve symptoms.
Q: How can we get new moms to talk about pain and pooping?
A: Get the word out! We used to not even talk about breastfeeding! It’s hard to reach new moms at such a new stage in life. Their hormones have changed, they’re returning to work, and everything has changed.
Advice: Avoid running and jumping for 3-6 months following childbirth. Be slow and patient with your body and with recovery. Take care of yourself!
Q: What can be done pre-delivery to prevent pain with sex?
A: Research currently focuses on stretching during the delivery process. Saint Mary’s hospital currently focuses on this research. There is a focus on increasing movement and flexibility of tissue during and prior to childbirth.

Q: Will having a hysterectomy affect my future sex function?
A: We try to leave a woman’s ovaries until age 65 to help with libido. It appears that many ovarian cancers start at the end of a woman’s tubes, so tube removal is generally a better option. Hysterectomies can shorten vaginal length, which can affect sex in addition to remaining scar tissue.
Q: What causes prolapse?
A: Prolapse is multifactorial.
Risk factors: The most critical is age, the second most critical is the number of vaginal deliveries a woman has had, followed by the number of deliveries in general, and finally a woman’s family history. When I’m seeing patients, I immediately ask about family history of prolapse to determine whether a woman’s symptoms will worsen.
Q: What do you do with vaginismus (muscle spasms around the vagina making sex painful)?
A: Sometimes a traumatic delivery can cause this to occur. I often use muscle relaxants and vaginal and anal valium to treat it (which have less side effects than if taken orally).
—————————————————————————————————
To schedule an initial evaluation with a pelvic floor physical therapist, you may contact Women’s Health Physical Therapy by phone: 804-379-3002 or email: whptrichmond@gmail.com
To schedule an appointment with Dr. Tovia Smith, you may call Virginia Women’s Center at: 804-288-4084





 Guest Blogger: Wilma Langeveld is a Dutch educated physical therapist who now lives in the United States. She specializes in connective tissue massage, cranio-sacral and Bowen therapy, lymph drainage, various techniques of massage and nutrition.
Guest Blogger: Wilma Langeveld is a Dutch educated physical therapist who now lives in the United States. She specializes in connective tissue massage, cranio-sacral and Bowen therapy, lymph drainage, various techniques of massage and nutrition.




 A: I.C. means a patient is consistently trying to achieve an empty bladder. This patient generally believes she has consistent UTI’s but no evidence of infection, bladder cancer, etc. This is a diagnosis of exclusion because many times the problem can only be identified by the treatments that don’t work. For example, I can exclude the possibility of overactive bladder syndrome if I prescribe antihistamines at night time and it doesn’t improve symptoms.
A: I.C. means a patient is consistently trying to achieve an empty bladder. This patient generally believes she has consistent UTI’s but no evidence of infection, bladder cancer, etc. This is a diagnosis of exclusion because many times the problem can only be identified by the treatments that don’t work. For example, I can exclude the possibility of overactive bladder syndrome if I prescribe antihistamines at night time and it doesn’t improve symptoms.